Rosuvastatin Drug: Indication, Dosage, Precaution, Side Effect , Storage, Category Type and corresponding Brands - www.genericdrugscan.com
Rosuvastatin
Drug Status in USA : ApprovedDrug Status in Canada : Approved
pronunciation
pronounced as (roe soo'' va stat' in)
Why is this medication prescribed?
Rosuvastatin is used together with diet, weight-loss, and exercise to reduce the risk of heart attack and stroke and to decrease the chance that heart surgery will be needed in people who have heart disease or who are at risk of developing heart disease. Rosuvastatin is also used to decrease the amount of cholesterol such as low-density lipoprotein (LDL) cholesterol ('bad cholesterol') and triglycerides in the blood and to increase the amount of high-density lipoprotein (HDL) cholesterol ('good cholesterol') in the blood. Rosuvastatin may also be used to decrease the amount of cholesterol and other fatty substances in the blood in children and teenagers 10 to 17 years of age who have familial heterozygous hypercholesterolemia (an inherited condition in which cholesterol cannot be removed from the body normally). Rosuvastatin is in a class of medications called HMG-CoA reductase inhibitors (statins). It works by slowing the production of cholesterol in the body to decrease the amount of cholesterol that may build up on the walls of the arteries and block blood flow to the heart, brain, and other parts of the body.
Accumulation of cholesterol and fats along the walls of your arteries (a process known as atherosclerosis) decreases blood flow and, therefore, the oxygen supply to your heart, brain, and other parts of your body. Lowering your blood level of cholesterol and fats with rosuvastatin has been shown to prevent heart disease, angina (chest pain), strokes, and heart attacks.
How should this medicine be used?
Rosuvastatin comes as a tablet to take by mouth. It is usually taken once a day with or without food. Take rosuvastatin at around the same time every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take rosuvastatin exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Your doctor will probably start you on a low dose of rosuvastatin and gradually increase your dose, not more than once every 2 to 4 weeks.
Continue to take rosuvastatin even if you feel well. Do not stop taking rosuvastatin without talking to your doctor.
What are the precautions to be followed?
Before taking rosuvastatin,- tell your doctor and pharmacist if you are allergic to rosuvastatin, any other medications, or any of the ingredients in rosuvastatin tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: anticoagulants ('blood thinners') such as warfarin (Coumadin); colchicine (Colcrys); cimetidine (Tagamet); cyclosporine (Neoral, Sandimmune); eltrombopag (Promacta); ketoconazole (Nizoral); other medications for high cholesterol such as fenofibrate (Tricor), gemfibrozil (Lopid), and niacin (Niaspan, Niacor); certain HIV protease inhibitors including atazanavir (Reyataz) taken with ritonavir (Norvir), and lopinavir and ritonavir (Kaletra); and spironolactone (Aldactone). Many other medications may also interact with rosuvastatin, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- if you are taking aluminum and magnesium hydroxide antacids (Mylanta, Maalox), take them at least 2 hours after rosuvastatin.
- tell your doctor if you have liver disease. Your doctor will order laboratory tests to see how well your liver is working even if you do not think you have liver disease. Your doctor will probably tell you not to take rosuvastatin if you have liver disease or if the tests show that you may be developing liver disease.
- tell your doctor if you are Asian, if you drink more than 2 alcoholic beverages daily, if you are 65 years of age or older, if you have ever had liver disease, or if you have or have ever had seizures, muscle aches or weakness, low blood pressure, or kidney or thyroid disease.
- tell your doctor if you are pregnant or plan to become pregnant. You should not become pregnant while you are taking rosuvastatin. Talk to your doctor about birth control methods that you can use during your treatment. If you become pregnant while taking rosuvastatin, call your doctor immediately. Rosuvastatin may harm the fetus.
- do not breastfeed while taking rosuvastatin.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking rosuvastatin. If you are hospitalized due to serious injury or infection, tell the doctor who treats you that you are taking rosuvastatin.
- ask your doctor about the safe use of alcoholic beverages while you are taking rosuvastatin. Alcohol can increase the risk of serious side effects.
What are possible side effects of this medication ?
Rosuvastatin may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:- constipation
- stomach pain
- dizziness
- difficulty falling asleep or staying asleep
- depression
- joint pain
- headache
- memory loss or forgetfulness
- confusion
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately or get emergency medical help:
:- muscle pain, tenderness, or weakness
- lack of energy
- fever
- chest pain
- yellowing of the skin or eyes
- dark colored urine
- pain in the upper right part of the abdomen
- nausea
- extreme tiredness
- weakness
- unusual bleeding or bruising
- loss of appetite
- flu-like symptoms
- rash
- hives
- itching
- difficulty breathing or swallowing
- swelling of the face, throat, tongue, lips, eyes, hands, feet, ankles, or lower legs
- hoarseness
Rosuvastatin may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
How to store the medication and dispose it of after its use later?
Keep this medication in the container it came in, tightly closed, and out of reach of children. Store it at room temperature and away from excess heat and moisture (not in the bathroom).
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program.
Drug Category/Class
- Hydroxymethylglutaryl-CoA Reductase Inhibitors
- HMG CoA Reductase Inhibitors
- Lipid Modifying Agents, Plain
- Lipid Modifying Agents
- Cardiovascular System
- Cytochrome P-450 CYP2C9 Inhibitors
- Cytochrome P-450 CYP2C9 Inducers
- Cytochrome P-450 CYP2C19 Inducers
- CYP3A4 Inhibitors
- HMG CoA reductase inhibitors
- HMG CoA reductase inhibitors in combination with other lipid modifying agents
| Prescribed | Used as an adjunct to dietary therapy to treat primary hyperlipidemia (heterozygous familial and nonfamilial), mixed dyslipidemia and hypertriglyce... |
| Weight : | 481.538 |
| Structure | Rosuvastatin |
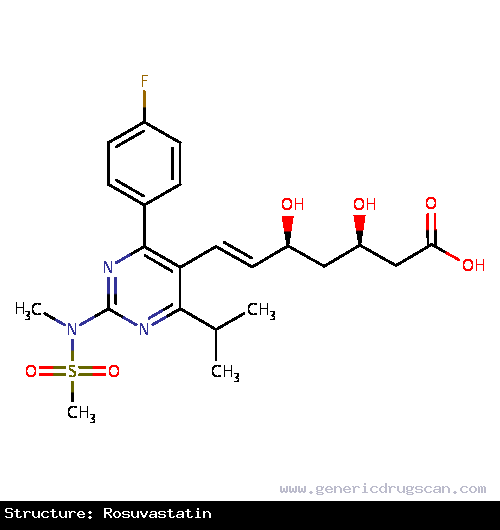 | |
| Formula | C22H28FN3O6S |
Rosuvastatin has 117 Brands listed
Search Generic Drugs alphabetically
