Oxcarbazepine Drug: Indication, Dosage, Precaution, Side Effect , Storage, Category Type and corresponding Brands - www.genericdrugscan.com
Oxcarbazepine
Drug Status in USA : ApprovedDrug Status in Canada : Approved
pronunciation
pronounced as (ox car baz' e peen)
Why is this medication prescribed?
Oxcarbazepine is used alone or in combination with other medications to control certain types of seizures. Oxcarbazepine is in a class of medications called anticonvulsants. It works by decreasing abnormal electrical activity in the brain.
How should this medicine be used?
Oxcarbazepine comes as a tablet and a suspension (liquid) to take by mouth. It is usually taken every 12 hours (twice a day) with or without food. Take oxcarbazepine at around the same times every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take oxcarbazepine exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Shake the suspension well right before each use to mix the medication evenly. Use the oral dosing syringe that came with the medication to withdraw the right amount of suspension from the bottle. You can swallow the suspension straight from the syringe or you can mix it with a small glass of water and swallow the mixture. Wash the syringe with warm water and allow it to dry thoroughly after use.
Your doctor will probably start you on a low dose of oxcarbazepine and gradually increase your dose, not more often than once every 3 days. If you were taking another medication to treat your seizures and are switching to oxcarbazepine, your doctor may gradually decrease your dose of the other medication while increasing your dose of oxcarbazepine. Follow these directions carefully and ask your doctor if you are not sure how much medication you should take.
Oxcarbazepine may help control your seizures but will not cure your condition. Continue to take oxcarbazepine even if you feel well. Do not stop taking oxcarbazepine without talking to your doctor, even if you experience side effects such as unusual changes in behavior or mood. If you suddenly stop taking oxcarbazepine, your seizures may get worse. Your doctor will probably decrease your dose gradually.
Your doctor or pharmacist will give you the manufacturer's patient information sheet (Medication Guide) when you begin treatment with oxcarbazepine and each time you refill your prescription. Read the information carefully and ask your doctor or pharmacist if you have any questions. You can also visit the Food and Drug Administration (FDA) website (http://www.fda.gov/Drugs) or the manufacturer's website to obtain the Medication Guide.
What are the precautions to be followed?
Before taking oxcarbazepine:- tell your doctor and pharmacist if you are allergic to oxcarbazepine, carbamazepine (Carbatrol, Epitol, Equetro, Tegretol), any other medications, or any of the inactive ingredients in oxcarbazepine tablets or suspension. Ask your pharmacist for a list of the inactive ingredients in oxcarbazepine tablets or suspension.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention any of the following: amiodarone (Cordarone); amitriptyline (Elavil); calcium channel blockers such as amlodipine (Norvasc), diltiazem (Cardizem, Dilacor, Tiazac), felodipine (Plendil), isradipine (DynaCirc), nicardipine (Cardene), nifedipine (Procardia), nimodipine (Nimotop), nisoldipine (Sular), and verapamil (Calan, Covera, Isoptin, Verelan); chlorpromazine (Thorazine);clomipramine (Anafranil); cyclophosphamide (Cytoxan, Neosar); desmopressin (DDAVP, Minirin, Stimate); diazepam (Valium); diuretics ('water pills'); hormonal contraceptives (birth control pills, rings, patches, implants, injections, and intrauterine devices); indapamide (Natrilix); other medications for seizures such as carbamazepine (Carbatrol, Epitol, Equetro, Tegretol), phenobarbital, phenytoin (Dilantin), and valproic acid (Depakene, Depakote); proton-pump inhibitors such as lansoprazole (Prevacid), omeprazole (Prilosec), and pantoprazole (Protonix); theophylline (Theo-Dur); and selective serotonin reuptake inhibitors (SSRIs) such as citalopram (Celexa), duloxetine (Cymbalta), escitalopram (Lexapro), fluoxetine (Prozac, Sarafem), fluvoxamine (Luvox), paroxetine (Paxil), and sertraline (Zoloft). Other medications may interact with oxcarbazepine, so be sure to tell your doctor and pharmacist about all the medications you are taking, even those that do not appear on this list. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had kidney or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you are using hormonal contraceptives, you should know that this type of birth control may not work well when used with oxcarbazepine. Hormonal contraceptives should not be used as your only method of birth control while you are taking this medication. Talk to your doctor about birth control methods that will work for you. Call your doctor if you miss a period or think you may be pregnant while you are taking oxcarbazepine.
- you should know that this medication may make you drowsy or dizzy, or may cause vision changes. Do not drive a car or operate machinery until you know how this medication affects you.
- remember that alcohol can add to the drowsiness caused by this medication.
- you should know that your mental health may change in unexpected ways and you may become suicidal (thinking about harming or killing yourself or planning or trying to do so) while you are taking oxcarbazepine for the treatment of epilepsy, mental illness, or other conditions. A small number of adults and children 5 years of age and older (about 1 in 500 people) who took anticonvulsants such as oxcarbazepine to treat various conditions during clinical studies became suicidal during their treatment. Some of these people developed suicidal thoughts and behavior as early as one week after they started taking the medication. There is a risk that you may experience changes in your mental health if you take an anticonvulsant medication such as oxcarbazepine, but there may also be a risk that you will experience changes in your mental health if your condition is not treated. You and your doctor will decide whether the risks of taking an anticonvulsant medication are greater than the risks of not taking the medication. You, your family, or your caregiver should call your doctor right away if you experience any of the following symptoms: panic attacks; agitation or restlessness; new or worsening irritability, anxiety, or depression; acting on dangerous impulses; difficulty falling or staying asleep; aggressive, angry, or violent behavior; mania (frenzied, abnormally excited mood); talking or thinking about wanting to hurt yourself or end your life; withdrawing from friends and family; preoccupation with death and dying; giving away prized possessions; or any other unusual changes in behavior or mood. Be sure that your family or caregiver knows which symptoms may be serious so they can call the doctor if you are unable to seek treatment on your own.
What are possible side effects of this medication ?
Oxcarbazepine may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:- dizziness
- drowsiness
- vision changes
- double vision
- fast, repeating eye movements that you cannot control
- diarrhea
- constipation
- heartburn
- stomach pain
- loss of appetite
- changes in the way food tastes
- dry mouth
- weight gain
- shaking of a part of the body that you cannot control
- difficulty coordinating movements
- falling down
- slowed movements or thoughts
- speech problems
- forgetfulness
- difficulty concentrating
- nervousness
- mood swings
- back pain
- muscle weakness or sudden tightness
- acne
- toothache
- earache
- hot flushes
- increased sweating
- cold symptoms
- nosebleed
- swelling, redness, irritation, burning, or itching of the vagina
- white vaginal discharge
- swelling of the face, throat, tongue, lips, eyes, hands, feet, ankles, or lower legs
- seizures that last longer or happen more often than in the past
- headache
- unusual thirst
- nausea
- vomiting
- weakness
- confusion
- decreased alertness
- rash
- bumps or blisters in the mouth, on skin, or genitals
- red or purple-colored blotches or dots on skin
- red, irritated eyes
- itching
- fever
- swollen glands in the neck or under the arms
- yellowing of the skin or eyes
- unusual bruising or bleeding
- bleeding from the rectum or blood in stools
- sore throat, cough, chills, and other signs of infection
- increased, decreased, or painful urination
- joint pain
- chest pain
How to store the medication and dispose it of after its use later?
Keep this medication in the container it came in, tightly closed, and out of reach and sight of children. Store it at room temperature and away from excess heat and moisture (not in the bathroom). Dispose of any unused suspension 7 weeks after the bottle is first opened.
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program.
Drug Category/Class
- Anticonvulsants
- Voltage-Gated Sodium Channel Blockers
- Nervous System
- Antiepileptics
- Carboxamide Derivatives
- Cytochrome P-450 CYP3A Inducers
- Cytochrome P-450 CYP2C19 Inducers
- CYP3A4 Inhibitors
- Carboxamide derivatives
| Prescribed | For use as monotherapy or adjunctive therapy in the treatment of partial seizures in adults with epilepsy and as adjunctive therapy in the treatmen... |
| Weight : | 252.268 |
| Structure | Oxcarbazepine |
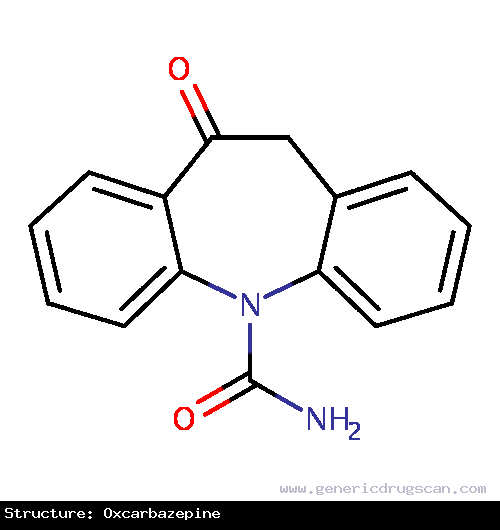 | |
| Formula | C15H12N2O2 |
Oxcarbazepine has 98 Brands listed
Search Generic Drugs alphabetically
