Moxifloxacin Drug: Indication, Dosage, Precaution, Side Effect , Storage, Category Type and corresponding Brands - www.genericdrugscan.com
Moxifloxacin
Drug Status in USA : ApprovedDrug Status in Canada : Approved
pronunciation
pronounced as (mox'' i flox' a sin)
Why is this medication prescribed?
Moxifloxacin is used to treat certain infections such as pneumonia, bronchitis, and sinus, skin, and abdominal (stomach area) infections caused by bacteria. Moxifloxacin is in a class of antibiotics called fluoroquinolones. It works by killing the bacteria that cause infections. Antibiotics will not work against colds, flu, or other viral infections.
How should this medicine be used?
Moxifloxacin comes as tablet to take by mouth. It is usually taken with or without food once a day for 5 to 21 days. The length of treatment depends on the type of infection being treated. Your doctor will tell you how long to take moxifloxacin. Take moxifloxacin at around the same time every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take moxifloxacin exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
You should begin to feel better during the first few days of treatment with moxifloxacin. If your symptoms do not improve or if they get worse, call your doctor.
Take moxifloxacin until you finish the prescription, even if you feel better. Do not stop taking moxifloxacin without talking to your doctor unless you experience certain serious side effects listed in the IMPORTANT WARNING and SIDE EFFECTS sections. If you stop taking moxifloxacin too soon or if you skip doses, your infection may not be completely treated and the bacteria may become resistant to antibiotics.
What are the precautions to be followed?
Before taking moxifloxacin,- tell your doctor and pharmacist if you are allergic or have had a severe reaction to moxifloxacin, other quinolone or fluoroquinolone antibiotics such as ciprofloxacin (Cipro), gatifloxacin (Tequin) (not available in the U.S.), gemifloxacin (Factive), levofloxacin (Levaquin), lomefloxacin (Maxaquin) (not available in the U.S.), nalidixic acid (NegGram), norfloxacin (Noroxin), ofloxacin (Floxin), and sparfloxacin (Zagam) (not available in the U.S.), or any other medications.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention the medications listed in the IMPORTANT WARNING section and any of the following: anticoagulants ('blood thinners') such as warfarin (Coumadin, Jantoven); certain antidepressants; antipsychotics (medications to treat mental illness); nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin, others) and naproxen (Aleve, Naprosyn, others); cisapride (Propulsid) (not available in the U.S.); diuretics ('water pills'); erythromycin (E.E.S., E-Mycin, Erythrocin, others); or certain medications for irregular heartbeat including amiodarone (Cordarone), disopyramide (Norpace), procainamide (Procanbid), quinidine, and sotalol (Betapace, Betapace AF, Sorine). Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- take moxifloxacin at least 4 hours before or at least 8 hours after you take any of these medications: antacids containing magnesium or aluminum (Maalox, Mylanta, Tums, others); didanosine (Videx); sucralfate (Carafate); or vitamin supplements that contain iron or zinc.
- tell your doctor if you or anyone in your family has or has ever had a prolonged QT interval (a rare heart problem that may cause irregular heartbeat, fainting, or sudden death) or an irregular heartbeat, and if you have or have ever had nerve problems, cerebral arteriosclerosis (narrowing of blood vessels in or near the brain that can lead to stroke or mini-stroke), seizures, chest pain, a slow heartbeat, a low level of potassium in your blood, or liver disease.
- tell your doctor if you are pregnant or plan to become pregnant or if you are breast-feeding. If you become pregnant while taking moxifloxacin, call your doctor.
- you should know that moxifloxacin may cause dizziness and lightheadedness. Do not drive a car, operate machinery, or participate in activities requiring alertness or coordination until you know how moxifloxacin affects you.
- plan to avoid unnecessary or prolonged exposure to sunlight or ultraviolet light (tanning beds and sunlamps) and to wear protective clothing, sunglasses, and sunscreen. Moxifloxacin may make your skin sensitive to sunlight. Call your doctor if you develop skin redness or blisters during your treatment with moxifloxacin.
What are possible side effects of this medication ?
Moxifloxacin may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:- nausea
- vomiting
- stomach pain
- diarrhea
- constipation
- gas
- heartburn
- loss of appetite
- change in ability to taste food
- sores in the mouth or on the tongue
- white patches in the mouth
- dry mouth
- headache
- weakness
- sweating
- vaginal itching or burning
- severe diarrhea (watery or bloody stools) that may occur with or without fever and stomach cramps (may occur up to 2 months or more after your treatment)
- dizziness
- confusion
- nervousness
- agitation
- restlessness
- not trusting others or feeling that others want to hurt you
- depression
- thinking about harming or killing yourself
- hallucinations (seeing things or hearing voices that do not exist)
- difficulty falling asleep or staying asleep
- nightmares
- uncontrollable shaking of a part of the body
- rash
- hives
- itching
- peeling or blistering of the skin
- fever
- swelling of the eyes, face, mouth. lips, tongue, throat, hands, feet, ankles or lower legs
- hoarseness
- difficulty breathing or swallowing
- fast heartbeat
- fainting
- loss of consciousness
- yellowing of the skin or eyes
- dark urine
- decreased urination
- seizures
- unusual bruising or bleeding
- joint or muscle pain
Moxifloxacin may cause problems with bones, joints, and tissues around joints in children. Moxifloxacin should not be given to children younger than 18 years old.
Moxifloxacin may cause nerve damage that may not go away even after you stop taking moxifloxacin. This damage may occur soon after you begin taking moxifloxacin. If you experience any of the following symptoms, call your doctor immediately: numbness, tingling, pain, or burning in the arms or legs; or a change in your ability to feel light touch, pain, heat, or cold. If you experience these symptoms, do not take any more moxifloxacin until you talk to your doctor. Your doctor may prescribe a different antibiotic for you to take instead of moxifloxacin.
Talk to your doctor about the risks of taking moxifloxacin or giving moxifloxacin to your child.
Moxifloxacin may cause other side effects. Call your doctor if you have any unusual problems while you are taking this medication.
How to store the medication and dispose it of after its use later?
Keep this medication in the container it came in, tightly closed, and out of reach of children. Store it at room temperature and away from excess heat and moisture (not in the bathroom).
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program.
Drug Category/Class
- Quinolones
- Fluoroquinolones
- Quinolone Antibacterials
- Antibacterials for Systemic Use
- Antiinfectives for Systemic Use
- Antiinfectives
- Quinolone and Quinoxaline Antibacterials
- Topoisomerase II Inhibitors
- Anti-Bacterial Agents
- Ophthalmologicals
- Sensory Organs
- Fluoroquinolones
| Prescribed | For the treatment of sinus and lung infections such as sinusitis, pneumonia, and secondary infections in chronic bronchitis. Also for the treatment... |
| Weight : | 401.4314 |
| Structure | Moxifloxacin |
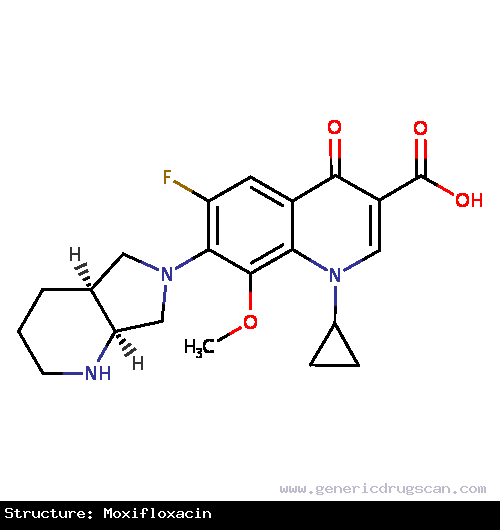 | |
| Formula | C21H24FN3O4 |
Moxifloxacin has 72 Brands listed
Search Generic Drugs alphabetically
