Leflunomide Drug: Indication, Dosage, Precaution, Side Effect , Storage, Category Type and corresponding Brands - www.genericdrugscan.com
Leflunomide
Drug Status in USA : ApprovedDrug Status in Canada : Approved
pronunciation
pronounced as (le floo' na mide)
Why is this medication prescribed?
Leflunomide is used alone or in combination with other medications to treat rheumatoid arthritis (a condition in which the body attacks its own joints, causing pain, swelling, and loss of function). Leflunomide is in a class of medications called disease-modifying antirheumatic drugs (DMARDs). It works by decreasing inflammation and slowing the progress of the condition, which can help improve the physical activity of people with rheumatoid arthritis.
How should this medicine be used?
Leflunomide comes as a tablet to take by mouth. It is usually taken once a day. Your doctor may tell you to take a larger dose of leflunomide for the first 3 days of treatment. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take leflunomide exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Your doctor may need to decrease your dose or stop treatment if you experience certain severe side effects. Be sure to tell your doctor how you are feeling during your treatment.
Leflunomide may help control the symptoms of your rheumatoid arthritis but does not cure it. Continue to take leflunomide even if you feel well. Do not stop taking leflunomide without talking to your doctor.
What are the precautions to be followed?
Before taking leflunomide,- tell your doctor and pharmacist if you are allergic to leflunomide, teriflunomide (Aubagio), any other medications, or any of the ingredients in leflunomide tablets. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what other prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention the medications listed in the IMPORTANT WARNING section and any of the following: anticoagulants ('blood thinners') such as warfarin (Coumadin Jantoven); cholestyramine (Prevalite); gold compounds such as auranofin (Ridaura); medications to treat cancer; other medications that suppress the immune system such as azathioprine (Azasan, Imuran), cyclosporine (Gengraf, Neoral, Sandimmune), sirolimus (Rapamune), and tacrolimus (Astagraf, Prograf); penicillamine (Cuprimine, Depen), and tolbutamide. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had serious infections or if you frequently get infections, cancer or other conditions affecting the bone marrow or the immune system (including human immunodeficiency virus
- HIV
- AIDS
- tell your doctor if you are breastfeeding. Do not breastfeed while you are taking leflunomide.
- if you are planning to father a child, you should talk to your doctor about stopping leflunomide and receiving a treatment to help to remove this medication from your body more quickly.
- ask your doctor about the safe use of alcoholic beverages while you are taking leflunomide.
- Taking leflunomide may decrease your ability to fight infection. Tell your doctor if you have an infection now or if you have any signs of infection such as fever, cough, or flu-like symptoms. If you experience any of the following symptoms during your treatment with leflunomide, call your doctor: fever; sore throat; cough; flu-like symptoms; area of warm, red, swollen, or painful skin; painful, difficult, or frequent urination; or other signs of infection. Your treatment with leflunomide may need to be interrupted if you have an infection.
- You may already be infected with tuberculosis (TB; a serious lung infection) but not have any symptoms of the disease. In this case, leflunomide may make your infection more serious and cause you to develop symptoms. Tell your doctor if you have or have ever had TB, if you have lived in or visited a country where TB is common, or if you have been around someone who has or has ever had TB. Before you begin your treatment with leflunomide, your doctor will perform a skin test to see if you have TB. If you do have TB, your doctor will treat this infection with antibiotics before you begin taking leflunomide.
- do not have any vaccinations without talking to your doctor.
- you should know that leflunomide may cause high blood pressure. You should have your blood pressure checked before starting treatment and regularly while you are taking this medication.
What are possible side effects of this medication ?
Leflunomide may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:- diarrhea
- vomiting
- heartburn
- headache
- dizziness
- weight loss
- back pain
- muscle pain or weakness
- pain, burning, numbness, or tingling in the hands or feet
- hair loss
- leg cramps
- dry skin
- rash with or without a fever
- hives
- blisters or peeling of skin
- mouth sores
- itching
- difficulty breathing
- new or worsening cough
- chest pain
- pale skin
Receiving medications which suppress the immune system may increase the risk of developing certain types of cancer. An increase in cancers was not reported in clinical studies with leflunomide to date. Talk to your doctor about the risks of receiving leflunomide.
Leflunomide may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
How to store the medication and dispose it of after its use later?
Keep this medication in the container it came in, tightly closed, and out of reach of children. Store it at room temperature and away from excess heat and moisture (not in the bathroom) and light.
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program.
Drug Category/Class
- Antirheumatic Agents
- Enzyme Inhibitors
- Adjuvants
- Selective Immunosuppressants
- Antineoplastic and Immunomodulating Agents
- Immunosuppressive Agents
- Cytochrome P-450 CYP1A2 Inhibitors
- Cytochrome P-450 CYP2C9 Inhibitors
- Cytochrome P-450 CYP1A2 Inducers
- Cytochrome P-450 CYP2C9 Inducers
- Selective immunosuppressants
| Prescribed | For the management of the signs and symptoms of active rheumatoid arthritis (RA) to improve physical function and to slow the progression of struct... |
| Weight : | 270.2073 |
| Structure | Leflunomide |
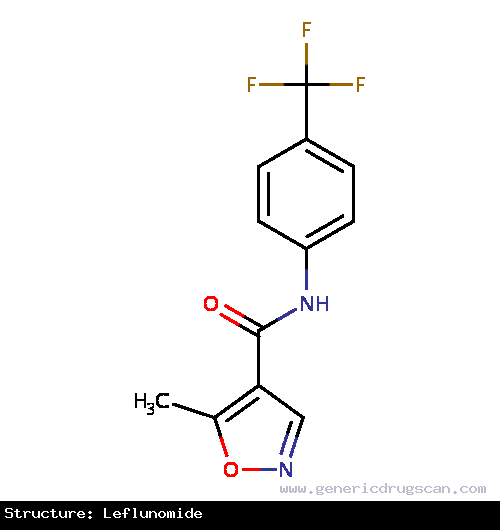 | |
| Formula | C12H9F3N2O2 |
Leflunomide has 18 Brands listed
Search Generic Drugs alphabetically
