Glipizide Drug: Indication, Dosage, Precaution, Side Effect , Storage, Category Type and corresponding Brands - www.genericdrugscan.com
Glipizide
Drug Status in USA : Approvedpronunciation
pronounced as (glip' i zide)
Why is this medication prescribed?
Glipizide is used along with diet and exercise, and sometimes with other medications, to treat type 2 diabetes (condition in which the body does not use insulin normally and, therefore, cannot control the amount of sugar in the blood). Glipizide is in a class of medications called sulfonylureas. Glipizide lowers blood sugar by causing the pancreas to produce insulin (a natural substance that is needed to break down sugar in the body) and helping the body use insulin efficiently. This medication will only help lower blood sugar in people whose bodies produce insulin naturally. Glipizide is not used to treat type 1 diabetes (condition in which the body does not produce insulin and, therefore, cannot control the amount of sugar in the blood) or diabetic ketoacidosis (a serious condition that may occur if high blood sugar is not treated).
Over time, people who have diabetes and high blood sugar can develop serious or life-threatening complications, including heart disease, stroke, kidney problems, nerve damage, and eye problems. Taking medication(s), making lifestyle changes (e.g., diet, exercise, quitting smoking), and regularly checking your blood sugar may help to manage your diabetes and improve your health. This therapy may also decrease your chances of having a heart attack, stroke, or other diabetes-related complications such as kidney failure, nerve damage (numb, cold legs or feet; decreased sexual ability in men and women), eye problems, including changes or loss of vision, or gum disease. Your doctor and other healthcare providers will talk to you about the best way to manage your diabetes.
How should this medicine be used?
Glipizide comes as tablets and extended-release (long-acting) tablets to take by mouth. The regular tablet is usually taken one or more times a day, 30 minutes before breakfast or meals. The extended-release tablet is usually taken once a day with breakfast. To help you remember to take glipizide, take it around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take glipizide exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Your doctor will probably start you on a low dose of glipizide and gradually increase your dose if needed. After you have taken glipizide for some time, glipizide may not control your blood sugar as well as it did at the beginning of your treatment. Your doctor may adjust the dose of your medication as needed so that the medication will work best for you. Be sure to tell your doctor how you are feeling and if your blood sugar test results have been higher or lower than normal at any time during your treatment.
Swallow the extended-release tablets whole. Do not chew, divide, or crush the tablets.
Glipizide helps control blood sugar but does not cure diabetes. Continue to take glipizide even if you feel well. Do not stop taking glipizide without talking to your doctor.
Ask your pharmacist or doctor for a copy of the manufacturer's information for the patient.
What are the precautions to be followed?
Before taking glipizide,- tell your doctor and pharmacist if you are allergic to glipizide, any other medications, or any of the ingredients in glipizide. Ask your pharmacist for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to mention anticoagulants ('blood thinners') such as warfarin (Coumadin); aspirin and other nonsteroidal anti-inflammatory medications (NSAIDs) such as ibuprofen (Advil, Motrin) and naproxen (Aleve, Naprosyn); beta blockers such as atenolol (Tenormin), labetalol (Normodyne), metoprolol (Lopressor, Toprol XL), nadolol (Corgard), and propranolol (Inderal); calcium channel blockers such as amlodipine (Norvasc), diltiazem (Cardizem, Dilacor, Tiazac, others), felodipine (Plendil), isradipine (DynaCirc), nicardipine (Cardene), nifedipine (Adalat, Procardia), nimodipine (Nimotop), nisoldipine (Sular), and verapamil (Calan, Isoptin, Verelan); chloramphenicol; cimetidine (Tagamet); diuretics ('water pills'); fluconazole (Diflucan); hormone replacement therapy and hormonal contraceptives (birth control pills, patches, rings, implants, and injections); insulin or other medications to treat high blood sugar or diabetes; isoniazid (INH); MAO inhibitors such as isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Eldepryl, Emsam, Zelapar), and tranylcypromine (Parnate); medications for asthma and colds; medications for mental illness and nausea; miconazole (Monistat); niacin; oral steroids such as dexamethasone (Decadron, Dexone), methylprednisolone (Medrol), and prednisone (Deltasone); phenytoin (Dilantin); probenecid (Benemid); salicylate pain relievers such as choline magnesium trisalicylate, choline salicylate (Arthropan), diflunisal (Dolobid), magnesium salicylate (Doan's, others), and salsalate (Argesic, Disalcid, Salgesic); sulfa antibiotics such as co-trimoxazole (Bactrim, Septra); sulfasalazine (Azulfidine); and thyroid medications. Also be sure to tell your doctor or pharmacist if you stop taking any medications while taking glipizide. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had G6PD deficiency (an inherited condition causing premature destruction of red blood cells or hemolytic anemia); if you have hormone disorders involving the adrenal, pituitary, or thyroid gland; or if you have heart, kidney, or liver disease. If you are taking the extended-release tablet, tell your doctor if you have short bowel syndrome (a condition where part of the intestine has been removed by surgery, damaged by disease, or you were born without part of your intestines); you have narrowing or a blockage of the intestines; or if you have ongoing diarrhea.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking glipizide, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking glipizide.
- ask your doctor about the safe use of alcoholic beverages while you are taking glipizide. Alcohol may make the side effects of glipizide worse. Consuming alcohol while taking glipizide also rarely may cause symptoms such as flushing (reddening of the face), headache, nausea, vomiting, chest pain, weakness, blurred vision, mental confusion, sweating, choking, breathing difficulty, and anxiety.
- plan to avoid unnecessary or prolonged exposure to sunlight and to wear protective clothing, sunglasses, and sunscreen. Glipizide may make your skin sensitive to sunlight.
- ask your doctor what to do if you get sick, develop an infection or fever, experience unusual stress, or are injured. These conditions can affect your blood sugar and the amount of glipizide you may need.
What are possible side effects of this medication ?
This medication may cause changes in your blood sugar. You should know the symptoms of low and high blood sugar and what to do if you have these symptoms.Glipizide may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- diarrhea
- gas
- feeling jittery
- dizziness
- uncontrollable shaking of a part of the body
- red or itchy skin
- rash
- hives
- blisters
- yellowing of the skin or eyes
- light-colored stools
- dark urine
- pain in the upper right part of the stomach
- unusual bruising or bleeding
- fever
- sore throat
Glipizide may cause other side effects. Call your doctor if you have any unusual problems while you are taking this medication.
In one study, people who took a medication similar to glipizide to treat their diabetes were more likely to die of heart problems than people who were treated with insulin and diet changes. Talk to your doctor about the risks of taking glipizide.
How to store the medication and dispose it of after its use later?
Keep this medication in the container it came in, tightly closed, and out of reach of children. Store it at room temperature and away from excess heat and moisture (not in the bathroom). Throw away any medication that is outdated or no longer needed. Talk to your pharmacist about the proper disposal of your medication.
Drug Category/Class
- Cytochrome P-450 CYP2C9 Inhibitors
- Cytochrome P-450 CYP2C9 Inducers
- CYP3A4 Inhibitors
- Hypoglycemic Agents
- Sulfonylureas
- Blood Glucose Lowering Drugs, Excl. Insulins
- Drugs Used in Diabetes
- Alimentary Tract and Metabolism
- Sulfonylureas
| Prescribed | For use as an adjunct to diet for the control of hyperglycemia and its associated symptomatology in patients with non-insulin-dependent diabetes me... |
| Weight : | 445.535 |
| Structure | Glipizide |
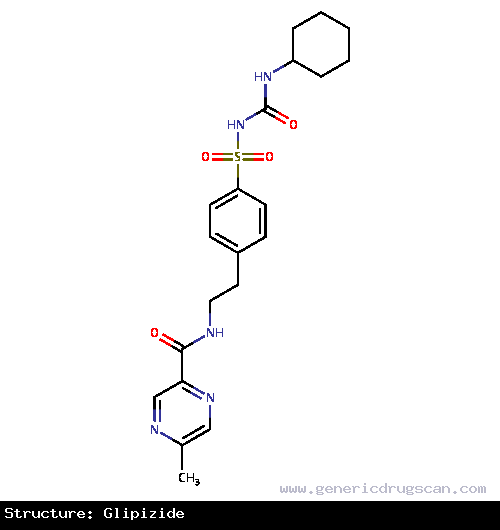 | |
| Formula | C21H27N5O4S |
Glipizide has 71 Brands listed
Search Generic Drugs alphabetically
